Our Approach
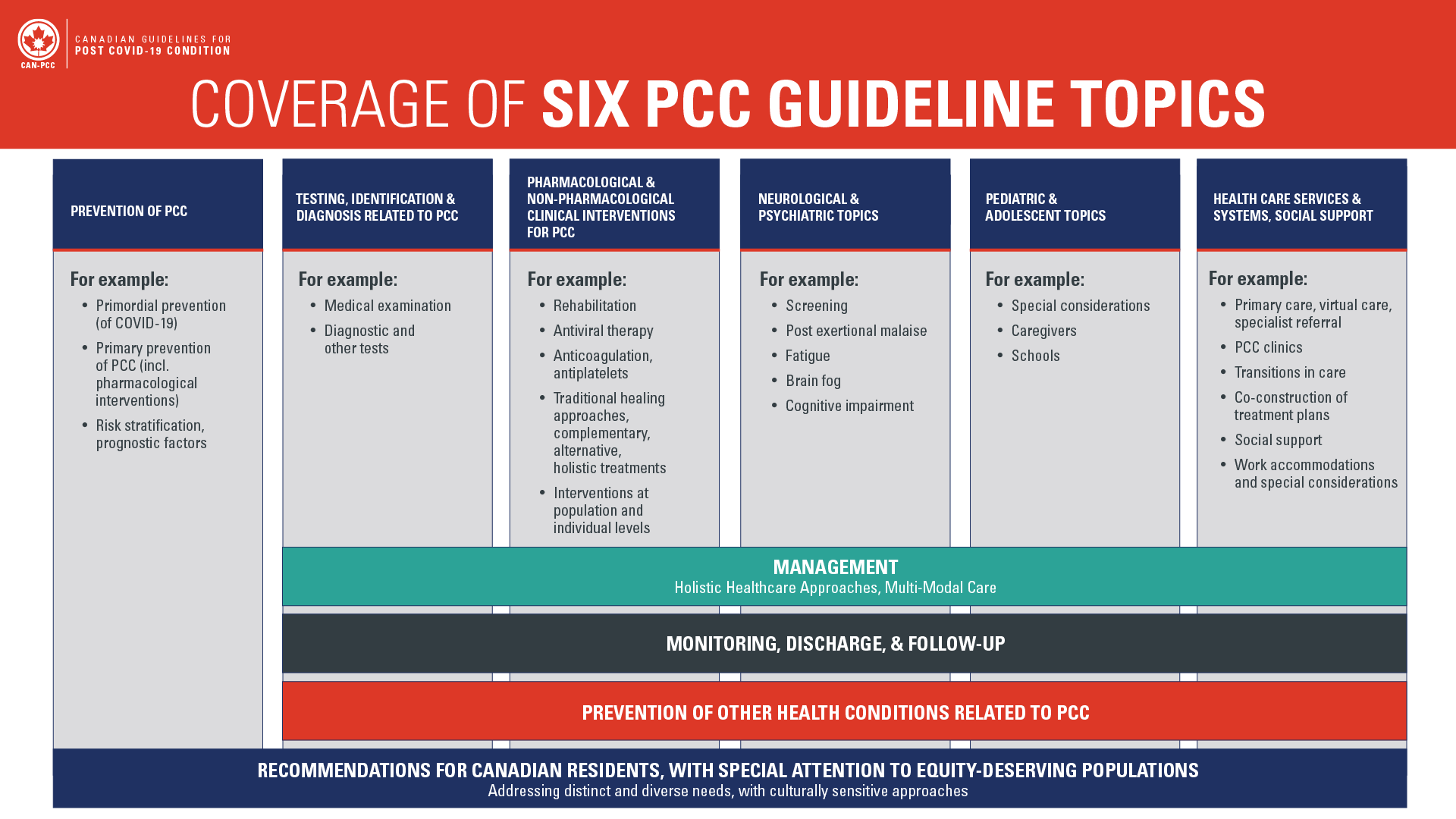
The Canadian Guidelines for Post COVID-19 Condition (CAN-PCC) aim to address 6 topic areas covering the full spectrum of PCC and health systems involved in supporting and managing this condition. A systematic, inclusive approach, with diverse consultation was used to prioritize 6 topics to meet the needs of Canada’s patients, health care system, and the public.
Expandable List
How did we prioritize and select the topics for the Canadian Guidelines for Post COVID-19 Condition?
Here are the steps that the CAN-PCC project team followed to prioritize topics:
Conduct a Scoping Review:
The CAN-PCC project team put together a comprehensive list of potential PCC topics, health conditions, and affected populations based on a scoping review of published literature on PCC.
Consultation with Interested Participants for Brainstorming and Generation of Priority Topics:
The team held brainstorming sessions during a project kick-off meeting with interested participants (i.e. patients, clinicians, researchers) to obtain input, add to the list of potential topics, refine and label topics, and clarify priority areas. At the end of the brainstorming sessions, a preliminary list of six topics was organized according to the top priorities and reviewed with the participants.
Public Consultation Survey:
The CAN-PCC project team developed and shared an online survey with the public to get their feedback about the suggested six guideline topics, identify any missing priority topic areas, and begin brainstorming potential guideline questions for the six topic areas.
Final Approval:
The CAN-PCC Guideline Development Group reviewed the public feedback from the survey, identified subtopic areas of priority, and gave final approval of the six guideline topics.
Scoping Review
To inform discussions on potential topics, guideline questions, PCC definitions, and target populations, we mapped and identified existing literature by conducting a scoping review. This review included a range of sources for the search, including Epistemonikos, the Cochrane Library, the World Health Organization’s COVID-19 Research database, the COVID-19 Evidence Network to support Decision-making (COVID-END) database, and the PCC Recommendations Map of Canada’s Drug and Health Technology Agency (CADTH).
We conducted the searches with help from research librarians. We included and extracted information from 24 published scoping reviews related to PCC, 37 systematic reviews focusing on the prevalence of health conditions and symptoms associated with PCC, and 34 published health guidelines addressing COVID-19 and PCC.
We extracted information to address our scoping review questions and reported: 1) a list of health conditions and symptoms experienced by individuals with PCC; 2) the prevalence data reported for these health conditions and symptoms; 3) a list of populations and population subgroups that were reported to be affected by PCC; and 4) an overview of interventions that have been evaluated in research studies for persons who have PCC, or are at risk of PCC.
Consultation with Interested Participants in Project Kick-off Meeting
Using the information from the scoping review as a basis for participant input, we conducted a two- day project kick-off workshop and engaged in small and large group discussions with approximately 110 individuals from interested groups, including members from the Canadian public, people with lived PCC experience, clinicians, and Canadian and international research collaborators. Through this collaborative exercise, which was facilitated by guideline methodologists, participants brainstormed and discussed priority topic areas, topics were organized and refined, and finally six priority guideline topics were identified: (1) Prevention of PCC, (2) Testing, Identification, and Diagnosis related to PCC, (3) Pharmacological and Non-pharmacological Clinical Interventions for PCC, (4) Neurological and Psychiatric Topics, (5) Pediatric and Adolescent Topics, (6) Healthcare Services and Systems, and Social Supports.
Public Consultation Survey
We captured many opinions and insights by conducting an online public consultation survey to assess agreement or disagreement with each of the suggested topics from the project kick-off workshop and invited suggestions for any missing priority areas. The survey was provided in both English and French with targeted promotion in all regions across Canada to ensure that the voices of a diverse range of individuals were heard and considered.
The Canadian Guidelines for Post COVID-19 Condition (CAN-PCC) team developed 11 Good Practice Statements (GPS) as a first step in the guideline development process. Here, we provide a brief overview of the key steps and considerations that were used for GPS development:
The members of the Guideline Development Group (GDG) and the six Guideline Teams (GTs) received training in the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology to develop GPS (see our Resources page for the methodology articles).
In summary, the framework for developing a GPS includes the following 5 criteria:
- The message is necessary in healthcare practice.
- Implementing the GPS results in a large net-positive consequence after consideration of all relevant outcomes and potential downstream consequences.
- Collecting and summarizing the evidence is a poor use of a guideline panel’s limited time, energy, or resources. The opportunity cost of collecting and summarizing the evidence is large and can be avoided.
- There is a well-documented clear and explicit rationale connecting the indirect evidence.
- The statement is clear and actionable.
- The GDG and GT members provided their declaration of interest (DOI) for independent assessment regarding relevant potential conflicts of interest (COI) by the Association of the Scientific Medical Societies in Germany (AWMF) using the COI policy. For these initial 11 GPS, the COI assessments addressed relevance for the specific GPS under consideration.
- The GTs drafted statements that met GPS criteria and were deemed important to promptly share with persons with lived PCC experience, health care professionals and care providers, policymakers, and the Canadian public.
- The draft GPS underwent a public comment period through an online survey, in English and French, which was shared with the Canadian public, as well as various Federal, Provincial and Territorial organizations and interested participants, and international collaborators. The survey collected feedback with respect to any concerns with the draft GPS, and suggestions for improvement.
The GDG discussed and together with the Guideline Teams made modifications to the GPS based on key issues identified form the feedback, including:
-
- Improvements in plain language use and consistent terminology across GPS, including for French language versions.
- Ensuring health equity considerations were adequately and consistently incorporated in the GPS.
- Keeping GPS and remarks concise to enhance uptake. More detailed relevant information, for example for implementation of the GPS, is available in the complete online GPS frameworks linked in the GPS and Recommendations List and Map.
- Ensuring that it was explicitly mentioned who should take the action, for example ‘health care professionals’ or ‘health educators’.
- Not focusing on domain-specific symptoms, such as neurological and cognitive changes, but addressing symptoms associated with PCC that cause limitations in daily activity. Specific symptoms will be addressed in upcoming formal recommendations.
- Not focusing on specific management options, but for example addressing the ‘plan of care’. Specific management options will be addressed in upcoming formal recommendations.
Final drafts of the GPS frameworks and statements provided by the Guideline Teams received approval for publication by the GDG.
Members of the CAN-PCC Collaborative, including the Guideline Development Group (GDG) and the six Guideline Teams (GTs,) submitted Declaration of Interest (DOI) forms to the Association of the Scientific Medical Societies in Germany (AWMF), which served to conduct an independent assessment of potential conflicts of interest (COI) for the CAN-PCC guidelines project. Both financial and non-financial disclosures were assessed following principles set out by the Guidelines International Network.
AWMF assessed potential COI at both the guideline topic and guideline question level. Upon assessment of disclosures, potential conflicts were classified as none, low, moderate, or high. Individuals with no COI had no limitations placed on their capacity as a member or leader of a guideline group. Individuals with low COI were not permitted to serve in a leadership capacity as guideline group co-chairs, but could otherwise participate fully in guideline development. Individuals with moderate COI were recused from making judgements or voting on recommendations on topics related to their COI, in addition to the limitations in place for those with low COI. Individuals with high COI were restricted from participating in discussions and making judgements or voting on recommendations related to their COI, in addition to the limitations in place for those with low and moderate COI. The assessed conflicts are reported for each GDG and GT member for all recommendations on the CAN-PCC RecMap. For additional details the full COI policy can be viewed here.
In Canada and across the world, some groups were disproportionately affected by Post COVID-19 Condition. These groups include but are not limited to women, elderly people in need of care and racialized groups.
To address the needs of these affected groups, we brought together an Equity Oversight Committee – one of the first guideline development projects to do so. The Equity Oversight Committee includes people with lived PCC experience, equity advocates and experts in equity methods. They work with different equity-seeking groups in Canada to incorporate a health equity lens in all stages of the guideline development process. For the guidelines, based on the literature, the committee selected certain equity-seeking groups to focus on.
This includes:
- Indigenous peoples
- Refugees/migrants
- 2SLGBTQIA+
- Elderly people in need of care
- Women
- Pregnant individuals
- Racialized groups
- Justice-involved people
- People with no fixed housing
- Rural and remote communities
- PICO specific populations at risk for disadvantage
The Equity Oversight Committee also uses two frameworks to integrate equity in the guidelines.
- The “Equity in Guidelines” framework outlines 7 steps to integrate equity from systematic reviews to inform the guidelines.
- A structured template to standardize integrating Equity in the Evidence to Decision (EtD) frameworks.
How did we select the questions to be addressed in the CAN-PCC guidelines and where can I find them?
Each recommendation we develop for the CAN-PCC guidelines should answer a healthcare question that leads to an action. These questions follow a format called “PICO,” which contains four key elements:
- Patient/Population: Who is the patient or population to whom this recommendation will apply?
- Intervention: What is the therapeutic or diagnostic intervention being evaluated?
- Comparison: What is the alternate intervention that is being compared?
- Outcomes: What are the desired health outcomes or effects of the intervention?
The CAN-PCC collaborative selected (“prioritized”) the most important health care questions related to PCC to be addressed by the recommendations. The selection process was based on a review of the research literature, as well as public consultation during our project kick-off and an online public survey asking for suggested questions. In December 2023, we published a draft version of the selected questions and sought public feedback about them. We also collected feedback from the Public Health Agency of Canada (PHAC), the Council of Chief Medical Officers of Health (CCMOH), and Federal, Provincial and Territorial interest holders. Our Guideline Teams and Guideline Development group discussed the public feedback and finalized the selection of the questions deemed to be of highest priority to address in the guidelines.
A final list of questions was developed, and they are grouped according to the six PCC topics.
It is critical that views and the perspective of the public and persons with lived experience are incorporated in the development of the CAN-PCC Guidelines. Below are four main ways we involve the public and persons with lived PCC experience in the CAN-PCC project:
CAN-PCC Working Groups
When forming the working groups, we ensured appropriate representation of people with lived PCC experience on each of our guideline teams, the guideline development group, and the equity oversight committee. To view our working group membership, please click here.
Public Member Panel
The Public Member Panel serves as one of the key CAN-PCC committees compromising of individuals who provide input on the guidelines from the perspective of people with lived PCC experience, carers for people with lived PCC experience, or members of the public. Their participation and input are captured through online surveys, focus groups, and review of documents when requested by the Guideline Teams
The roles of the public member panel include:
- Providing feedback on guideline development steps such as health outcome prioritization, input about patients’ values and preferences, and reviewing draft recommendation statements.
- Promoting awareness of the guideline development project and sharing requests for broader public input (e.g. during public comment periods for draft recommendations)
Public Comment Surveys
As part of public consultation using online surveys, we requested members of the public and persons with lived experience to provide their input on the guideline topics and guideline questions. We also hold consultation periods every month using an online survey to obtain feedback on draft recommendations as they are being developed. The feedback received is carefully reviewed by the guideline development group and guideline teams to finalize recommendations before publication.
If you are interested in participating in our public comment surveys, sign up for our newsletter here to be notified of our next public comment period.
Co-Designing CAN-PCC Resources
As part of our knowledge mobilization efforts, members of the public, such as through our Public Member Panel, will be involved in co-designing guideline resources and tools, including infographics and online resource sheets, that help to increase the accessibility, understanding, and use of the CAN-PCC guideline recommendations.
Learn more about how guidelines are developed


